HEALTH
Warning Signs: Is your tooth trying to tell you it needs a root canal?

Introduction to Root Canals: Understanding Your Dental Needs
Root canals are often misunderstood dental procedures that play an important role in maintaining oral health. When you think of a root canal, the immediate image might be discomfort or pain, but the reality is that a root canal can alleviate pain caused by an infected tooth and can save a tooth that might otherwise need to be extracted. As a trusted New York City dentist, Dr Sachar understands the importance of recognizing the early signs that indicate a root canal may be necessary. Being aware of these signs and getting treatment quickly can help improve the prognosis of a tooth treated with root acnal therapy. A root canal specialist or an experienced NYC Dentist can provide the necessary root canal treatment in one simple visit.
What is a Root Canal?
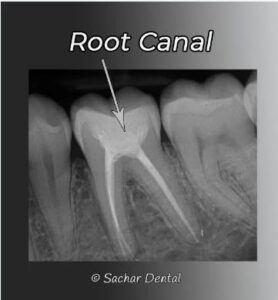
A root canal is a dental procedure designed to save a tooth that is severely infected or decayed. This treatment involves removing the infected pulp from inside the tooth, cleaning the root canal within the root, and then filling the canal and sealing it to prevent further infection. Despite common misconceptions, root canals are usually not painful , thanks to advances in dental techniques and anesthesia. The best NYC dentist will ensure the procedure is performed efficiently and comfortably, aiming to relieve pain and restore the tooth’s function. Root canals help maintain natural teeth, preventing the need for extractions and more complex procedures like implants or bridges, preserving your smile and overall oral health.
The pulp is the innermost part of the tooth, containing nerves and blood vessels, and when it becomes infected or inflamed, it can cause significant pain and discomfort. The root canal process involves removing the affected pulp, cleaning the inside of the root, and sealing it to prevent further infection.
Root canals are common procedures performed by dentists to save teeth that would otherwise be lost to decay or infection. At Sachar Dental NYC, our experienced team of NYC Dentist uses state-of-the-art technology to perform root canals efficiently and comfortably.
Once a root canal is completed, the tooth requires a permanent filling or a crown over it to give it strength.

Understanding Tooth Pain: Is It Time for a Root Canal?
One of the most common signs that you might need a root canal is persistent tooth pain. However, not all tooth pain indicates the need for a root canal. It is essential to understand the types of pain that suggest this procedure may be necessary:
- Severe Toothache: If you experience intense, throbbing pain that doesn’t go away, it could be a sign of infection within the tooth that may need root canal treatment.
- Sensitivity to Temperature: Increased sensitivity to hot foods and drinks can indicate that the tooth’s pulp is damaged. If the sensitivity lingers long after the temperature stimulus is removed, it might be time to visit your dentist.
- Swelling and Tenderness: Swelling in the gums near the affected tooth, along with tenderness, can indicate an infection that has spread from the tooth’s pulp. This is a warning sign that a root canal might be needed to stop the spread of infection.
Visible Signs: What to Look for in Your Mouth
In addition to pain and sensitivity, there are visible signs that might suggest the need for a root canal:
- Discoloration: A tooth that becomes darkened or discolored can signal damage or infection of the pulp. This can happen when the blood supply to the tooth is compromised, often requiring a root canal.
- Gum Pimples: Small, pimple-like bumps on the gums near a tooth can be a sign of an abscess, which occurs when an infection spreads from the pulp to the surrounding bone and tissue. An abscess often requires immediate attention and treatment through a root canal may ned needed.
- Loose Tooth: An adult tooth that feels loose may indicate that the pulp is infected, which can weaken the tooth’s support structure. A root canal may be needed and can help stabilize the tooth and prevent further issues.
The Root Canal Procedure: What to Expect
Understanding what to expect during a root canal procedure can help alleviate any anxiety you may have about the treatment. Here is an overview of the typical process:
Examination and Diagnosis
The first step in the root canal procedure is a thorough examination by an expert NYC dentist. The dentist will assess your symptoms, take X-rays, and diagnose the condition of the tooth to determine if a root canal is necessary.
Anesthesia
Before the procedure begins, the dentist will administer local anesthesia to numb the affected area and ensure you are comfortable throughout the treatment.
Pulp Removal
Once the area is numb, the dentist will create an opening in the tooth to access the infected pulp. The damaged pulp is carefully removed, and the interior of the tooth is cleaned and disinfected to eliminate any bacteria.
Filling and Sealing
After the pulp is removed, the dentist will fill the empty space with a biocompatible material and seal the tooth to prevent further infection. In some cases, a dental crown may be placed over the tooth to restore its strength and appearance.
Follow-Up Care
Following the procedure, your NYC dentist will provide instructions for post-treatment care and schedule a follow-up appointment to monitor your recovery and ensure the success of the root canal.
The Importance of Timely Treatment
Ignoring the signs that you might need a root canal can lead to more severe dental problems. Untreated infections can spread to other parts of the mouth, jaw, and even the bloodstream, leading to systemic infections. It is crucial to address these signs early by visiting a trusted New York City dentist like those at Sachar Dental NYC.
Preventing the Need for a Root Canal
While root canals are sometimes unavoidable, there are steps you can take to reduce the risk of needing one:
- Maintain Good Oral Hygiene: Brushing twice a day, flossing daily, and using mouthwash can help prevent decay and infection.
- Regular Dental Checkups: Visiting your NYC dentist regularly allows for early detection and treatment of dental issues before they progress.
- Avoid Hard Foods: Chewing on ice, hard candy, or other tough foods can crack your teeth and increase the risk of pulp inflammation and infection.
- Wear a Mouthguard: If you participate in sports, wearing a mouthguard can protect your teeth from injury.
Root Canal vs. Tooth Extraction
When faced with a severely damaged or infected tooth, patients often wonder whether a root canal or tooth extraction is the better option. While it is always better to save a tooth with a root canal, not all infected teeth are salvageable. Your dentist will be able to evaluate the tooth and its x-rays and see if a tooth can be saved withb a root canal or is an extraction necessary. If a tooth is extracted it can be replaced with a dental implant.
Myths About Root Canals: Separating Fact from Fiction
Many myths surround the root canal procedure, leading to unnecessary fear and anxiety. Let’s debunk some of these myths:
Myth: Root Canals Are Painful
Fact: With modern dental techniques and anesthesia, root canals today are not painful. The procedure is similar to getting a cavity filling. At Sachar Dental NYC, our team ensures patient comfort throughout the procedure.
Myth: Root Canals Cause Illness
Fact: There is no scientific evidence linking root canals to illness elsewhere in the body. The procedure is safe and effective for eliminating infection and preserving dental health.
Myth: Extracting the Tooth is Better
Fact: Preserving your natural teeth is always the best option when possible. A root canal allows you to keep your tooth and maintain its function, preventing the need for more invasive procedures like implants or bridges.
Why Choose Sachar Dental NYC for Your Root Canal?
When considering a root canal, it is important to choose a reputable and experienced NYC dentist. At Sachar Dental NYC, our team of skilled professionals, led by Dr. Sachar, is committed to providing the highest quality of care. We use the latest technology to ensure precise and effective treatment, minimizing discomfort and recovery time. If a root canal is complex, we will refer you to an endodontist whom we trust.
A Healthy Smile is a Phone Call Away
If you’re experiencing any of the warning signs mentioned above, don’t hesitate to contact Sachar Dental NYC at 212-752-1163. Our compassionate and skilled team is ready to help you achieve a pain-free and healthy smile.
Experience Quality Dental Care
At Sachar Dental NYC, we understand that the thought of a root canal can be daunting. However, our dedicated team is here to guide you through the process with care and expertise. Whether you need a root canal or other dental services, our New York City dentist office is equipped to provide top-notch dental care tailored to your needs.
Don’t let dental pain disrupt your life. Contact us today to schedule an appointment with Dr. Sachar and our team at Sachar Dental NYC. We are committed to ensuring your comfort and delivering exceptional dental care in the heart of NYC.
READ MORE about NYC Dentist for Root Canal Treatment on our services page.
More here.
Sachar Dental NYC
20 East 46th Street
Rm 1301
(Between 5th Ave & Madison Ave)
New York, NY 10017
212-752-1163
https://www.sachardental.com
HEALTH
How Plastic Surgery Can Boost Your Confidence

In contemporary society, confidence is a very important aspect in our personal as well as professional lives. A lot of people have had insecurity concerns when it comes to their physical appearances, which can have an effect on how they relate with other people, as well as how they see themselves. There are some individuals who have plastic surgery as a means to improve their physical appearances, which can help them develop confidence in the process as well. But how is confidence increased through plastic surgery?
Understanding the Connection Between Looks and Confidence
Physical appearance often affects our perception of ourselves. Sometimes our perception of flaws and imperfections in our body and facial features affects our own confidence and feelings about our appearance. Such insecurities can affect our behavior in social settings and our performances at work. For some people, it is a struggle to reconcile their appearance and feelings about that appearance.
Plastic surgery bridges the gap for people wishing to overcome specific physical issues. With the help of plastic surgery, people are able to synchronize their outward look with their inner self-perception. In other words, individuals who undergo the surgery can overcome their anxiety regarding their looks and increasing self worth.
How Plastic Surgery Addresses Personal Insecurities
Among the top reasons why people undergo plastic surgery is the correction of zones within their appearance that have long made them unhappy with what they look like. It could be a rhinoplasty to remake the shape of the nose. It could be a facelift to remove the signs of aging. It could be breast augmentation to improve the body’s proportions that have long had a detrimental effect on their confidence.
As people feel better about their appearance, they also notice that their self-esteem improves. This liberation from their own criticism encourages people to feel at ease with others and to be who they are without fear. This emotional shift can be as significant as the physical transformation itself for people.
Psychological Gains Independent of Physical Alterations
Even though the effects of plastic surgery are seen and felt physically, there are psychological gains that can be more dramatic. Plastic surgery patients feel empowered and more capable of taking charge of their lives. They can gain a feeling of accomplishment through their desired reconstruction.
In addition, the increased self-confidence may impact every sphere of life. That is, it may bring increased motivation towards personal and career goals, frequent trying of new experiences, and healthy relationships. The positive feedback associated with increased confidence often ripples way beyond the initial cosmetic change.
The Importance of Realistic Expectations
While plastic surgery is proven to offer considerable emotional and psychological relief, it must be considered from a realistic angle. Plastic surgery is not a cure for all worries and problems faced in life. It is only an aid in ensuring an individual feels connected to his or her ideal self-image.
Additionally, before arranging for plastic surgeries to be performed, one should have very open conversations with professional surgeons to learn more about the end results. A person who embarks on plastic surgeries, yet maintains a very level-headed perspective throughout the process, stands to gain the most benefits concerning confidence.
Plastic Surgery as a Means of Moving Towards Self-Care
The decision to undertake plastic surgery should also be recognized as a form of self-care. This is because undertaking plastic surgery indicates that one is actually investing in their well-being. The decision to prioritize these aspects of one’s well-being indicates that they have finally turned a new leaf.
The motives for undergoing plastic surgery can represent significant aspects of personal growth and self-awareness. It is the realization that it is necessary to feel good and look good in order to be happy. When people treat themselves with kindness and respect, including through cosmetic enhancements, it contributes to a healthier relationship with their self-image.
Overcoming Social Stigmatisms of Plastic Surgery
While plastic surgery has indeed grown in popularity, there remains a degree of associated social stigma. Misconceptions regarding vanity or superficiality may prevent those who could genuinely benefit from the associate improvement in their quality of life. Nevertheless, attitudes are changing with more and more people realizing the mental health benefits associated with cosmetic interventions.
By talking about plastic surgery as a confidence booster, many would be judged less and more understanding. Self-confidence is a very personal thing, and everyone has the right to be comfortable and happy in their own skin, whatever way they feel that is attained.
Plastic Surgery Embracing Confidence
Plastic surgery may make important contributions to confidence through responses to physical insecurity and even psychological treatments. It is not a cure, but the right operation, with realistic expectations, can help individuals feel more consistent with their self-image and empowered to participate in life fully.
Ultimately, confidence comes from accepting and loving oneself, and for some, plastic surgery is an important and valuable part of that process. If people take good care of themselves and make smart choices, then they can use plastic surgery as a tool that can help inspire a renewed sense of self-worth.
HEALTH
Winter Care for Women: Preventing UTIs and Vaginal Infections

Introduction
Winter and high pollution periods can influence daily habits and natural immunity, increasing the risk of urinary tract and vaginal infections in women. Colder temperatures often lead to reduced water intake, layered clothing, prolonged indoor stays and changes in hygiene practices, all of which may affect urogenital health. At the same time, seasonal stress, lack of sunlight and lowered immunity can make the body more susceptible to bacterial and fungal infections.
Why Does Winter Raise UTI and Vaginal Infection Risk?
Winter can affect daily habits and body defences, increasing infection risk. The following factors contribute to this rise.
- Behavioural Drivers: People may drink less water in cold weather and delay urination, increasing bacterial concentration in urine. Tight, non-breathable clothing and dampness after exercise trap moisture and encourage microbial growth.
- Physiological Factors: Seasonal viral infections, poor sleep and stress may reduce immune strength in the urogenital tract. Reduced indoor humidity may cause dryness and micro-abrasions that allow infection.
- Environmental Contributors: Pollution may increase inflammation and weaken mucosal defence. Together, these factors explain the seasonal rise in cystitis and vaginal infections.
Common Conditions and What They Mean
Understanding common winter-related infections helps in early detection and treatment.
- Uncomplicated Lower UTI (Cystitis): Sudden urinary frequency, urgency, burning sensation and cloudy or strong-smelling urine. Needs timely care to prevent spread to kidneys.
- Pyelonephritis (Upper UTI): Fever, flank pain and nausea suggest kidney involvement and require urgent attention.
- Vulvovaginal Candidiasis: Itching, thick white discharge and discomfort; often linked to moisture, antibiotic use or diabetes.
- Bacterial Vaginosis: Thin grey discharge with a fishy odour, caused by an imbalance of vaginal bacteria.
- Sexually Transmitted Infections (STIs): May present with abnormal discharge and require targeted testing and partner treatment.
Prevention Checklist – Practical Winter Measures That Work
Before implementing preventive steps, it is important to understand how daily habits can influence infection risk.
- Hydration and Regular Voiding: Sip fluids throughout the day and avoid holding urine for long periods.
- Clothing and Hygiene: Wear breathable cotton underwear, avoid tight synthetic garments for long hours and change damp clothes promptly.
- Toilet Care: Wipe front to back and avoid douching or scented products that disturb natural flora.
- Post-Sex Habits: Urinate after intercourse, avoid irritants and use barrier protection when required.
- Manage Comorbidities: Maintain blood sugar if diabetic and complete full antibiotic courses when prescribed.
- Environmental Measures: Use indoor humidifiers to prevent dryness and shower after exposure to pollution.
- Proactive Health Behaviours: If infections recur, speak with a gynaecologist or women’s health specialist about preventive options.
When to Consult a Gynaecologist or Seek Urgent Care?
You should book a gynaecologist near me or women’s health specialist near me via Apollo 24|7 if you have fever with urinary symptoms, flank pain, persistent symptoms despite initial treatment, recurrent UTIs, severe vaginal discomfort or symptoms of an STI. Seek urgent care for high fever, severe flank pain, vomiting, dizziness or signs of sepsis. Teleconsultation may help with early guidance and referral if needed.
You may also consult a gynaecologist in Kolkata through Apollo 24|7 when symptoms persist or worsen.
What a Specialist Will Do – Diagnostic and Management Approach
During consultation, the specialist follows a stepwise evaluation and treatment process.
- Initial Tests: Urine dipstick, microscopy, urine culture if needed and vaginal swabs for candida, BV or STIs.
- Further Evaluation: Renal ultrasound or CT for suspected complicated infections; bladder scan or urodynamics for voiding issues.
- Treatment Approach: Simple cystitis may need empirical treatment. Vaginal infections like candidiasis and BV receive topical or oral medication. Recurrent cases require tailored therapy and sometimes multidisciplinary care.
- Follow-Up: Symptom review, advice on prevention and referral to urology if structural issues are suspected.
Preparing for Your Appointment on Apollo 24|7
Before your consultation, be ready with your medical details.
- Have Ready: Symptom timeline, recent test reports, current medications, allergies, pregnancy status and any imaging results.
- Booking Tips: Search terms such as gynaecologist near me, best gynaecologist near me, gynaecologists near me, best gynaecologists near me or women’s health specialist near me can help find suitable options.
- What to Expect: A clear diagnosis plan, treatment if required and personalised prevention advice. The specialist will guide if in-person tests are necessary.
Conclusion
Winter may increase the risk of UTIs and vaginal infections due to lower immunity, reduced hydration and lifestyle changes. Most infections are preventable with simple habits like staying hydrated, maintaining hygiene and wearing breathable clothing. If symptoms recur or do not improve, consulting a gynaecologist near me via Apollo 24|7 ensures timely diagnosis and proper care. Early medical attention helps avoid complications and supports better comfort and health during the colder months.
HEALTH
Minimally Invasive Thyroid Nodule Treatments Available in Singapore

Thyroid nodules are a common clinical finding, and while most are benign, they can cause discomfort, aesthetic concerns, or, in rare cases, indicate malignancy. In Singapore, the rise of routine health screenings has led to increased detection of thyroid nodules, and patients are often concerned about invasive surgery, scarring, and recovery time. Fortunately, minimally invasive thyroid nodule treatments offer effective alternatives that reduce downtime while delivering precise outcomes.
As an endocrinologist practicing in Singapore, I frequently see patients seeking guidance on safe and efficient nodule management. Understanding the range of treatment options, their benefits, and limitations is crucial for making informed decisions.
Understanding Thyroid Nodules
A thyroid nodule is a growth or lump in the thyroid gland, located in the neck just below the Adam’s apple. Nodules vary in size, composition, and clinical significance. They may be solid or fluid-filled (cystic) and can present as a single nodule or multiple nodules. While the majority are benign, features such as rapid growth, suspicious ultrasound characteristics, or abnormal lab results warrant further investigation.
Patients often experience anxiety upon discovery of a nodule. The first step is a thorough evaluation, including physical examination, thyroid function tests, and imaging studies such as ultrasound. This assessment guides the choice of treatment, from observation to minimally invasive interventions.
For patients seeking thyroid nodule treatment Singapore, it’s important to understand that not all nodules require surgery. Many can be managed effectively with targeted, minimally invasive procedures that preserve thyroid function and minimize complications.
When Minimally Invasive Treatments Are Appropriate
Minimally invasive interventions are typically recommended for:
- Symptomatic benign nodules causing discomfort, difficulty swallowing, or breathing issues.
- Cystic or predominantly cystic nodules that recur after aspiration.
- Nodules with cosmetic concerns, particularly when located in the visible areas of the neck.
- Patients wishing to avoid conventional surgery or those unsuitable for general anesthesia.
The decision depends on nodule size, type, symptoms, and patient preference. In Singapore, advanced imaging and procedural techniques allow endocrinologists to tailor treatment plans safely and effectively.
Common Minimally Invasive Treatments
1. Ultrasound-Guided Fine Needle Aspiration (FNA)
FNA is both a diagnostic and therapeutic tool. A thin needle is used under ultrasound guidance to extract cells from the nodule for cytological examination. While primarily diagnostic, FNA can also provide temporary relief for cystic nodules by aspirating fluid, reducing nodule size and pressure symptoms.
2. Radiofrequency Ablation (RFA)
Radiofrequency ablation is a cutting-edge technique widely used in Singapore. RFA delivers thermal energy through a thin electrode inserted into the nodule under ultrasound guidance, causing controlled tissue destruction. Over weeks to months, the treated nodule shrinks significantly, alleviating symptoms without the need for surgical removal.
RFA is particularly effective for solid and mixed nodules. Advantages include:
- Preservation of normal thyroid tissue.
- Minimal scarring, as the procedure is performed percutaneously.
- Short recovery time, often allowing patients to resume daily activities immediately.
3. Laser Ablation
Laser ablation uses focused light energy to coagulate nodule tissue. Similar to RFA, it is performed under ultrasound guidance and is suitable for nodules causing cosmetic or functional concerns. Laser ablation provides precise control over the treated area, minimizing damage to surrounding tissue.
4. Ethanol Ablation (Ethanol Injection)
Ethanol ablation involves injecting concentrated alcohol into cystic or predominantly cystic nodules, inducing fibrosis and shrinkage. This approach is highly effective for recurrent cysts and is minimally invasive, performed under local anesthesia in an outpatient setting.
5. High-Intensity Focused Ultrasound (HIFU)
HIFU is an emerging non-invasive technique that uses focused ultrasound energy to heat and destroy nodule tissue without any needle puncture. While still less common than RFA or laser ablation, HIFU is ideal for patients who prefer completely non-invasive treatment.
Advantages of Minimally Invasive Treatments
Minimally invasive interventions offer several benefits over conventional surgery:
- Reduced Recovery Time: Most patients can return to normal activities within a day or two.
- Preservation of Thyroid Function: Unlike surgery, which may require partial or total thyroid removal, these treatments preserve healthy tissue.
- Minimal Scarring: Small puncture sites or no incisions reduce visible scarring.
- Lower Risk of Complications: There is reduced risk of nerve injury, infection, and bleeding compared to open surgery.
Patient Considerations and Follow-Up
Although minimally invasive procedures are highly effective, patients should understand that results may vary depending on nodule size and type. Repeat treatments may occasionally be required, especially for larger nodules.
Regular follow-up includes ultrasound monitoring and thyroid function tests to ensure the nodule shrinks appropriately and to detect any new growth. In Singapore, clinics offering these treatments often provide comprehensive follow-up care, ensuring patient safety and long-term outcomes.
Lifestyle and Supportive Measures
While medical intervention is the cornerstone of treatment, supportive measures can enhance outcomes:
- Maintaining a balanced diet rich in iodine, vitamins, and minerals to support thyroid health.
- Avoiding excessive neck trauma or strain.
- Monitoring for symptoms such as neck swelling, voice changes, or difficulty swallowing.
Educating patients about their condition and providing reassurance are integral to successful management. Many patients experience anxiety upon nodule detection, and clear communication about treatment options, benefits, and risks can alleviate concerns.
Choosing a Specialist in Singapore
Selecting an experienced endocrinologist or thyroid specialist is critical. Clinics that specialize in thyroid care offer advanced diagnostic tools, procedural expertise, and personalized treatment plans.
For patients seeking thyroid nodule treatment in Singapore, it’s important to choose a provider who can assess whether minimally invasive techniques are appropriate and who can guide you through every step of the process.
Conclusion
Minimally invasive thyroid nodule treatments provide effective, safe, and cosmetically favorable alternatives to conventional surgery. In Singapore, advancements such as RFA, laser ablation, ethanol injection, and HIFU have revolutionized care, allowing patients to address nodules efficiently while minimizing downtime and preserving thyroid function.
Ultimately, early detection, proper evaluation, and individualized treatment planning are key to optimal outcomes. With expert guidance and minimally invasive interventions, patients can manage thyroid nodules confidently, achieving both functional and aesthetic satisfaction.
-

 TECHNOLOGY7 months ago
TECHNOLOGY7 months agoTop 10 Must-Read Stories from Kristen Archives You Can’t Miss
-
 TECHNOLOGY1 year ago
TECHNOLOGY1 year agoSky Bri Net Worth Revealed: How She Built Her Financial Empire
-

 TOPIC1 year ago
TOPIC1 year agoBasement Renovation Contractors: How They Tackle Structural Issues During Renovations
-

 TOPIC9 months ago
TOPIC9 months ago5 Reasons the //Vital-Mag.Net Blog Dominates Lifestyle
-

 TOPIC8 months ago
TOPIC8 months agoTop 10 Articles from the ://Vital-Mag.net Blog That You Can’t Miss
-

 BEAUTY1 year ago
BEAUTY1 year agoRevitalize Your Hair with Oribe Hair Care for Damaged Hair: Style It with Blue Dresses for Weddings and Events
-

 CRYPTO11 months ago
CRYPTO11 months agoCrypto30x.com Review: Is It the Right Platform for You?
-

 BUSINESS7 months ago
BUSINESS7 months agoTraceLoans Explained What You Need to Know
