HEALTH
How Can You Identify Panic Attacks Through Physical Symptoms?

Have you ever felt your heart racing for no clear reason? Maybe your chest felt tight, or it suddenly became hard to breathe. Panic attacks can be frightening, especially when they come out of nowhere.
Many people don’t realize they’re experiencing a panic attack because the symptoms feel so physical. It can seem like a heart problem or another medical emergency. Understanding these signs can help you recognize a panic attack and take steps to manage it.
Rapid Heartbeat and Chest Pain
One of the most common symptoms of a panic attack is a racing heart. It can feel like your heart is pounding too hard or too fast. Some people describe it as a fluttering feeling in their chest. This can be scary, especially when combined with chest pain.
The pain from panic attacks does not continue beyond a short period, but heart attack pain will persist. The signs and symptoms most often appear during periods of anxiety instead of during physical movements. It’s important to seek medical evaluation if you’re unsure about your symptoms.
Shortness of Breath and Dizziness
During panic attacks, the overwhelming sensation makes it seem impossible to obtain enough oxygen to breathe. The quickening of your breathing becomes noticeable as well as sensations of choking. The quickness of your breathing causes hyperventilation which makes your brain send signals that result in dizziness and lightheadedness.
When the body reacts to stress, it generates these symptoms. Body preparations initiate through brain signals, triggering defensive responses even when no real danger exists. With that, treatment options for panic disorder can manage these reactions, especially when scarce breathing due to fear worsens respiratory difficulties.
Sweat and Chills
Sweating appears as a common indicator of panic attacks in numerous people. A panic attack can develop within seconds regardless of air temperature conditions. Individuals either sweat everywhere on their bodies or experience only their hands and forehead becoming moist during panic attacks. When the body activates its natural response for “fight or flight,” it enters this state of alarm because of fear.
A subset of panic attack sufferers feel tense as their bodies produce shivers when under stress. The body generates goosebumps while also feeling cold when the environmental temperature remains warm. The body reacts to these physical alterations as a result of stress hormone activity.
Shaking and Muscle Tension
Shaking and trembling serve as frequent symptoms that appear during panic attacks. The body parts which experience tension include the hands as well as legs and can extend to become widespread throughout the entire body. Electrical signals in the muscles can create a sensation of weakness in some individuals.
Muscle tension is also common. Most individuals experience their shoulders becoming stiff together with jaw tightness and taut muscles in their stomach area. The body starts preparing protective measures although there is no actual threat present.
Nausea and Stomach Problems
Panic attacks can affect the stomach in many ways. Some people feel queasy, while others experience stomach cramps. A sudden urge to use the bathroom can also happen. This is because the brain and digestive system are closely linked.
When stress levels rise, the stomach reacts. Some people with frequent panic attacks even develop digestive issues like irritable bowel syndrome (IBS). Learning to manage anxiety can help reduce these stomach problems.
Feeling Detached or Unreal
A strange but common panic attack symptom is a sense of unreality. Some people feel like they are watching themselves from the outside. Others say the world around them seems distant or dreamlike. This feeling is called depersonalization or derealization.
It happens because the brain is overwhelmed by fear and stress. To protect itself, it tries to “shut off” certain sensations. Even though this feeling can be frightening, it is temporary. Once the panic attack ends, everything returns to normal.
Tingling or Numbness
Panic attacks can cause tingling in the hands, feet, face, or other body parts. Some people also feel numbness, especially in their fingers or lips. This happens because rapid breathing changes the balance of oxygen and carbon dioxide in the blood.
Though it may feel alarming, this sensation is not harmful. Breathing slowly and deeply can help bring the body back to normal.
Sudden Fear of Losing Control
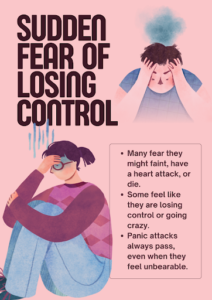
One of the most distressing panic attack symptoms is the intense fear that something terrible is about to happen. Some people worry they will faint, have a heart attack, or even die. Others feel like they are going crazy or losing control of their mind.
This fear can be overwhelming, but it is a normal part of panic attacks. It happens because the brain misinterprets physical symptoms as signs of danger. The good news is that panic attacks always pass, even when they feel unbearable in the moment.
Weakness and Fatigue
After a panic attack, many people feel exhausted. The body has been on high alert, using up a lot of energy. This can leave muscles feeling weak and the mind feeling drained.
Some people need to rest after an attack, while others feel shaky. Drinking water and focusing on slow breathing can help the body recover quickly.
Recognizing and Managing Panic Attacks
Understanding these symptoms is the first step in managing panic attacks. When you know what is happening, it becomes easier to remind yourself that you are not in danger.
If panic attacks happen often, it may help to speak with a doctor or therapist. There are many ways to reduce their impact, from breathing exercises to therapy and medication. Learning how to manage anxiety can make a big difference in improving daily life.
Conclusion
Panic attacks can be overwhelming, but recognizing the physical symptoms can help you feel more in control. From a racing heart to dizziness and muscle tension, these signs may feel alarming but are not life-threatening.
Understanding how your body responds to stress makes it easier to manage panic when it happens. If panic attacks occur often, seeking support from a healthcare professional can provide helpful strategies. With the right tools, you can learn to reduce their impact and regain a sense of calm.
FAQs
Can panic attacks happen while sleeping?
Yes, panic attacks can occur during sleep, causing sudden waking with intense fear and physical symptoms like a racing heart and shortness of breath.
How long do panic attack symptoms usually last?
Most panic attacks peak within 10 minutes and last around 20 to 30 minutes, though some symptoms may linger longer.
Are panic attack symptoms the same for everyone?
No, symptoms can vary from person to person. Some may experience chest pain and dizziness, while others feel numbness or chills.
HEALTH
How Delayed Care After Surgery Can Lead to Dangerous Infections

Surgery is often seen as the peak of a patient’s medical journey, but in reality, healing begins after the incision is closed. What happens in the hours and days following a procedure can make all the difference between recovery and life-threatening complications. When patients are neglected during this critical window—when signs of infection are missed or care is delayed—the consequences can spiral into organ failure, sepsis, or even death.
Hospital-acquired infections are among the most preventable causes of injury in modern healthcare. Yet, delayed recognition and treatment continue to be leading contributors to catastrophic outcomes after surgery. In many cases, the danger isn’t in the operating room—it’s in the silence that follows. Patients and families who experience these tragedies often turn to legal advocates like Meinhart and Manning to hold negligent providers accountable and seek justice for harm that was never supposed to happen.
When Postoperative Monitoring Falls Short
Following surgery, patients should be closely observed for signs of infection, especially those who are immunocompromised or undergoing major procedures. Vital signs, wound appearance, fluid output, and pain levels all tell a story—but someone needs to be listening. When hospital staff fail to monitor changes or delay responding to concerns, minor symptoms can quickly escalate.
What begins as a low-grade fever or slight swelling may be dismissed as routine discomfort. But within hours, that “normal” post-op recovery can evolve into a raging infection. Early intervention is key—yet too many hospitals cut corners on staffing, leave patients in understaffed wards, or ignore the urgency flagged by nurses and families.
Warning Signs That Should Never Be Overlooked
When an infection starts, the body shows clear signs that something is wrong. Healthcare providers must recognize these signs and act quickly. Ignoring them can lead to serious and preventable problems. Key warning signs that need immediate medical attention include:
- Elevated heart rate which can indicate the body is under stress from an internal infection.
- Rapid or labored breathing is a sign of potential sepsis or respiratory distress.
- Confusion or disorientation is often a red flag for systemic infection, especially in older adults.
- Escalating pain at or near the wound or surgical site.
- Redness, swelling, or warmth that continues to spread around the wound.
- Pus or discharge from an incision or injury, especially if it has an odor.
- Fever or chills are common early symptoms of infection.
- Persistent fatigue or weakness that interferes with daily functioning.
The Cost of Hospital-Acquired Infections
Infections like MRSA, sepsis, and C. diff are known risks in hospital settings, yet many are still the result of poor hygiene, inadequate protocols, or delayed action. A single infection can lead to additional surgeries, amputations, or months of ICU care. For the patient, it often means prolonged pain, permanent disability, or, in the worst cases, death.
Beyond the physical toll, the emotional and financial burdens are immense. Families must deal with mounting medical bills, missed work, and the heartbreak of watching a loved one suffer. Infections that could have been prevented with prompt care are among the most painful types of malpractice because they are both common and avoidable.
When Providers Dismiss or Downplay Concerns
A critical failure in postoperative care is the tendency of some providers to downplay or deflect patients’ concerns. Complaints of pain, unusual discharge, or fatigue may be chalked up to a normal part of healing. But patients know their own bodies, and when they feel that something is wrong, their voices deserve to be taken seriously.
Delayed responses often stem from a culture of dismissiveness or hierarchy, where nurses feel unable to challenge doctors, and patients are left waiting for decisions from higher-ups. This lag in attention can make the difference between a course of antibiotics and a medical emergency. Empowering all team members to act on concerns is crucial, but when this system fails, accountability must follow.
Infection in the Shadow of Surgery
The public perception of surgery tends to focus on the technical skill of the operating physician. But the risk of infection isn’t just about what happens on the table—it’s about what happens next. Surgical wounds are highly vulnerable to bacteria, especially in hospitals where resistant strains thrive.
When sterile environments aren’t maintained, or dressings aren’t properly changed, bacteria can enter the body and multiply quickly. A delay of just 24 hours in identifying and treating a surgical infection can mean the difference between full recovery and permanent damage. The operating room may have been sterile, but it’s what happens in the recovery room that often determines the outcome.
The Tragedy of Sepsis and Septic Shock
One of the most devastating consequences of a delayed infection diagnosis is sepsis—a condition where the body’s response to infection spirals out of control. If untreated, it can lead to tissue damage, organ failure, and death. Time is everything. Once sepsis takes hold, every hour of delay increases mortality risk significantly.
Families often find themselves blindsided by the rapid decline: one day, the patient is recovering from surgery; the next, they are fighting for their life. Medical records reviewed in hindsight often show that warning signs were present but not acted upon. The tragedy isn’t just in the infection itself—it’s in the missed opportunity to stop it in time.
How Systemic Failures Contribute to Delay
It’s not always one person’s mistake that leads to delayed care—it’s often a cascade of failures. Charting errors, missed pages, short staffing, or a lack of standardized infection protocols can all contribute to delayed diagnosis and treatment. These aren’t isolated missteps—they reflect a system not designed to respond quickly to a crisis.
When hospitals prioritize efficiency or profit over patient safety, infections rise, and lives are put at risk. Legal claims not only address the damage to individual patients but also highlight dangerous systemic trends that need to be corrected. A lawsuit can become a call for broader reform that protects future patients from similar fates.
Seeking Accountability Through Legal Action
When a preventable infection changes a life forever or takes it, the pursuit of accountability becomes vital. Legal action gives families a voice when hospitals offer none. It allows them to ask: Why wasn’t my loved one monitored more closely? Why were the signs ignored? What policies were in place—and why didn’t they work?
Working with experienced attorneys ensures that these questions are not brushed aside. It opens the door to compensation for pain, medical bills, lost income, and more. But perhaps most importantly, it helps ensure that no other patient is left waiting in silence while an infection spreads. With legal advocacy, justice can do more than heal—it can prevent.
HEALTH
How Psychiatric Urgent Care Differs from Traditional ER Visits for Mental Health

Just as physical health emergencies, mental health crises can also occur at any moment and have to be taken care of as early as possible. But when individuals show up with acute psychiatric symptoms, such as severe anxiety, suicidality, or psychosis, they frequently go to emergency rooms (ERs) that are less than optimally constructed to address their needs.
This article discusses some of the major distinctions between psychiatric emergency care and typical emergency room visits, and how the two settings treat people with psychological distress.

The Environment
In contrast to receiving immediate therapy online, ERs are usually crowded, confusing, and full of patients with various health care emergencies, with some seriously ill patients (with fractured bones) and others (with heart attacks). To a person who is already in a weak mental state, such multi-sensory saturation may result in increased anxiety, confusion, or fearfulness.
Among the most obvious and evident contrasts between psychiatric urgent care centers and regular ERs, the atmosphere should be considered.
Typically, the location of the traditional ERs will have:
- High sound and shining lights
- Waiting rooms that are packed
- Mixture of medical emergencies (e.g., trauma and cardiac incidents)
- Stressful environment (both staff and patients)
In a contrasting manner, a psychiatric urgent care centers provide:
- Noise-free, relaxing, spacious rooms with semi-dim light and pale-colored walls
- Smaller rooms that offer respite where there is sensory overload (especially in the case of semi-private rooms )
- Easy chairs that will make one feel easy and relaxed
These design factors help in the provision of a therapeutic environment that allows de-escalation and stabilization of emotions. It is only this environment that can make serious contributions in the healing process before the actual treatment is given.
The Staff
Traditional ERs and psychiatric emergency care centers look extremely dissimilar in terms of personnel specialization and orientation.
In the conventional ERs, the workforce usually comprises:
- Doctors and nurses who work in emergencies
- General practitioners
- Poor or slow availability of psychiatric consultants
- Experts who practice mainly in physical health crises
The following are the staff members of psychiatric urgent care centers:
- Psychiatric nurse practitioners and psychiatrists
- Medical care, social workers, and therapists
- Crisis counselors for mental health crises
- Employees who perform trauma-informed care and de-escalation practices

Treatment Approach
Another important difference has to do with the care approach to a mental health crisis. In recent years, mental health disorders such as anxiety and bipolar disorder have increased by almost 40%.
A treatment in a classical ER can include:
- Stabilization and monitoring
- Use of medicine to treat the acute manifestation
- Referring to the external psychiatric services is usually done in an uncoordinated manner
- Scant or no treatment
The mental health urgent care centers shall usually provide:
- Full Psychiatric assessment
- On-the-spot therapy (individual, group, or family)
- Crisis management and short-term planning of treatment Short-term planning of treatment
- Psychiatric control of medication within the site itself
- Designing an integrated care plan
Wait Times and Accessibility
Delays to care and waiting lists in terms of patient outcomes can have an enormous impact on mental health emergencies.
In classic ERs, there is a possibility of:
- Wait time, especially when triaged behind physical emergencies
- Overcrowded mental health units with few resources
- Psychiatric services have limited availability of operating time
- Timecare barriers
The mental health ER can provide:
- Reduced wait times emphasized the psychiatric need
- Urgent mental health needs that can be accessed on a walk-in basis
- Evenings and weekends, as well as extended hours
- More time-effective contact with specialist personnel
Follow-Up Care
Continuity of care will be important in terms of delivering long-term stability and recovery following the initial crisis.
ERs tend to give little follow-up to include:
- General discharge prescriptions
- Referrals to community mental health care giver
- No definite form of continuity of care
- Potential loss of patients in the cracks
Psychiatric urgent care centers, such as those from Mindful Care, are preoccupied with:
- Discharge planning in detail
- Referring to continuing treatment and mental treatment
- Access to the community resources and groups of support
- In other instances, brief follow-up treatment or drug counselling
Conclusion
A major innovation in the practice of mental health crises is the psychiatric urgent care centers. Although traditional emergency rooms will always be an important resource to provide treatment to people in life-threatening or co-occurring physical emergencies, it is not always geared appropriately to address psychiatric emergencies fully.
Some of the strengths of psychiatric urgent care are:
- Mental wellness-sustaining environments: Specialist environments
- Specially hired mental healthcare workers within the organization
- Individual and instant treatment for mental health
- Less time and more coverage
- Enhanced continuity of care in the form of coordinated follow-up
Psychiatric urgent care constitutes care between outpatient behavioral therapy and inpatient hospitalization, acting as a middle ground, focuses on patient dignity, expertise, and early intervention. Better outcomes and a more humane mental health care process are the promise of this model to individuals, families, and communities.
HEALTH
Natural Ways to Support Oral Health Through Diet

Why Diet Matters for Oral Health
What you eat doesn’t just impact your weight and energy, it shapes your smile too. Nutrition plays a crucial role in teeth straightening and the health of your gums.
The mouth is the starting point of the digestive system, and it’s often one of the first places where nutritional imbalances show up. Deficiencies can weaken enamel, trigger inflammation, and increase your risk of gum disease. But a nutrient-rich, well-balanced diet does the opposite; it helps your body protect and rebuild.
In this blog, you will come to know about key nutrients that support oral health, foods that help clean your teeth naturally, the surprising impact of food texture on alignment, and how to support your smile while you sleep.
Nutrients That Strengthen Teeth and Gums
Let’s start with the essentials. Your teeth and gums need specific vitamins and minerals to stay strong and healthy, especially if you’re aiming for long-term oral wellness.
- Calcium and Phosphorus
These minerals help build and maintain enamel, the protective outer layer of your teeth. They also strengthen the jawbone, which holds your teeth in place.
Sources: dairy products like milk and yogurt, leafy greens, almonds, tofu, and fish like sardines. - Vitamin D
Even if you get enough calcium, your body won’t absorb it well without vitamin D. This nutrient also plays a role in reducing gum inflammation.
Sources: sunlight exposure, mushrooms, and fatty fish like salmon. - Vitamin C
Vital for gum health, vitamin C supports collagen production and protects against gum inflammation and bleeding.
Sources: citrus fruits, strawberries, bell peppers, broccoli, and kiwi. - Antioxidants
Antioxidants help protect your gums from oxidative stress and reduce the buildup of harmful bacteria.
Sources: green tea, blueberries, cranberries, dark chocolate, and spinach.
The Role of Food Texture in Jaw Development
The strength and alignment of your jaw aren’t genetic. The consistency of your food, especially during childhood, plays a huge role in shaping your facial structure.
Soft and processed foods require minimal chewing. Over time, this can lead to weaker jaw muscles and narrower dental arches. Harder fibrous foods require more effort and promote stronger jaws and better bone density.
Diet plays a significant role in jaw development. A well-aligned jaw supports straight bottom teeth, reducing the chances of dental crowding or orthodontic issues later in life.
In fact, a study published in the National Library of Medicine observed that children who regularly consumed harder, textured foods developed better mandibular control and chewing efficiency, indicating more robust muscle and bone development in the jaw.
Whole foods like raw carrots, celery, apples, sugar-free foods, and whole grain bread not only challenge your teeth, but they also help strengthen the muscles around them and encourage healthy oral posture.
Foods That Naturally Clean the Mouth
Some foods act like natural toothbrushes and mouthwash, helping reduce plaque, freshen breath, and support enamel without the need for chemicals.
- Crunchy fruits and vegetables
Raw apples, carrots, and celery scrub the surface of your teeth and stimulate saliva production, which helps wash away food particles and neutralize acids. - Water-rich foods
Cucumbers, melons, and leafy greens help keep the mouth hydrated and flush bacteria away. The more you chew them, the more saliva your mouth produces, which is your body’s first defense against decay. - What to avoid
Sugar, soda, processed starches, and acidic foods like citrus or vinegar-based snacks can erode enamel over time. Coffee and red wine can also stain teeth and dry out the mouth.
Every bite either helps or harms your oral environment. Choosing fibrous, water-dense foods can make a small but steady difference.
Nighttime Oral Health: Diet and Protection
Your mouth gets through a lot while you sleep. If you clench your jaw, breathe through your mouth, or eat too close to bedtime, your teeth may suffer. Fortunately, good nutrition can solve these problems
- Magnesium-rich foods
Magnesium helps relax muscles and nerves, which may reduce nighttime jaw tension or clenching.
Helpful options: almonds, bananas, avocados, pumpkin seeds, and leafy greens. - Hydration
Dry mouth at night increases the risk of cavities. Drinking water in the evening, especially after your last meal, helps prevent bacteria.
Using a night guard after a healthy evening diet can protect your teeth from grinding and erosion while you sleep. It creates a physical barrier and absorbs pressure from unconscious clenching, keeping your enamel safe and your jaw more relaxed.
While diet plays a supporting role, a night guard is often necessary for those dealing with bruxism or teeth grinding.
Bonus Tips for a Diet-Supported Oral Routine
Even the best diet needs good habits alongside it. Consistency in both food choices and habits is what ultimately makes the difference. These daily tips can enhance your efforts and help your smile last longer.
- Don’t brush right after acidic foods
Acid temporarily softens enamel, and brushing too soon can cause more damage. Wait at least 30 minutes. - Rinse after meals
If brushing isn’t possible after lunch or snacks, rinsing your mouth with water can help reduce food particles and acids. - Chew sugar-free gum
This stimulates saliva and may reduce dry mouth and bad breath. - Try saltwater rinses or oil pulling
While not replacements for brushing, they can be gentle supplements to your oral hygiene, especially if your gums feel sensitive. - Avoid constant snacking
Frequent eating, even of healthy foods, keeps your mouth in a low-level acidic state. Give your mouth breaks between meals.
Wrap Up
Healthy teeth aren’t just about toothpaste and dental visits. They are built every day, meal by meal. What you eat feeds the tissues, bones, and systems that support your smile.
By focusing on nutrient-dense foods, staying hydrated, choosing textures that challenge your jaw, and avoiding sugar overload, you create an oral environment that heals instead of deteriorates.
Whether you’re trying to maintain straight bottom teeth, reduce nighttime grinding with a night guard, or simply feel more confident in your smile, the food you choose matters more than you think.
It’s not about perfection. It’s about making smarter, more intentional choices every day. Because your mouth isn’t separate from your body, it’s the first part of your health journey.
Let it start with what’s on your plate.
-

 TECHNOLOGY2 weeks ago
TECHNOLOGY2 weeks agoTop 10 Must-Read Stories from Kristen Archives You Can’t Miss
-
 TECHNOLOGY6 months ago
TECHNOLOGY6 months agoSky Bri Net Worth Revealed: How She Built Her Financial Empire
-

 TOPIC8 months ago
TOPIC8 months agoBasement Renovation Contractors: How They Tackle Structural Issues During Renovations
-

 TOPIC3 months ago
TOPIC3 months ago5 Reasons the //Vital-Mag.Net Blog Dominates Lifestyle
-

 TOPIC1 month ago
TOPIC1 month agoTop 10 Articles from the ://Vital-Mag.net Blog That You Can’t Miss
-

 CRYPTO5 months ago
CRYPTO5 months agoCrypto30x.com Review: Is It the Right Platform for You?
-

 BUSINESS2 weeks ago
BUSINESS2 weeks agoTraceLoans Explained What You Need to Know
-

 BUSINESS4 weeks ago
BUSINESS4 weeks agoDecoding the Kennedy Funding Ripoff Report: Facts vs. Fiction
